Pregnancy comes with a lot of medical terminology that can feel overwhelming, especially when a diagnosis lands in your lap during a routine ultrasound. One condition that often catches parents off guard is placenta previa — a complication that affects roughly 1 in 200 pregnancies. While it sounds alarming, the good news is that with timely diagnosis and the supervision of an experienced gynecologist, placenta previa is entirely manageable — and most mothers go on to deliver healthy, beautiful babies.
What Is Placenta Previa?
The placenta is a remarkable organ that grows inside the uterus during pregnancy. It attaches to the uterine wall and acts as a lifeline between mother and baby — supplying oxygen, nutrients, and filtering waste products through the umbilical cord.
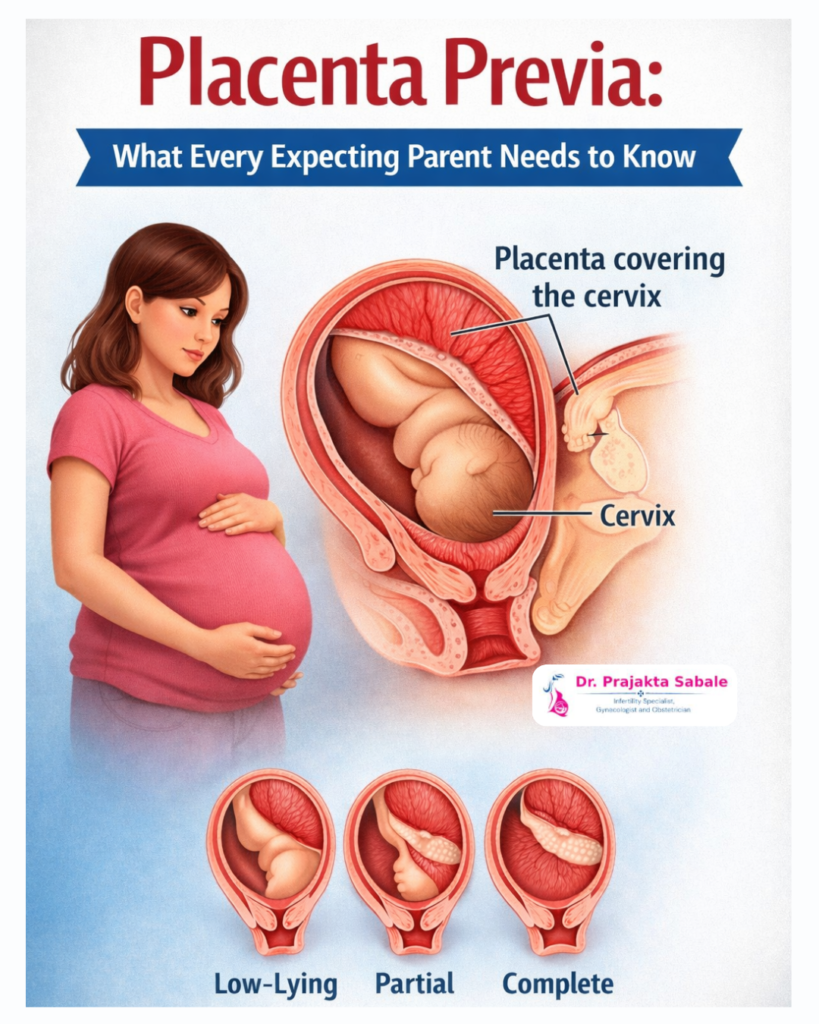
In a typical pregnancy, the placenta attaches to the upper portion of the uterus, well away from the cervix (the opening to the birth canal). In placenta previa, however, the placenta attaches low in the uterus and partially or completely covers the cervical opening.
This positioning creates a significant problem: if the cervix begins to dilate during labour — or even during the late stages of pregnancy — it can cause the placenta to bleed, posing serious risks to both mother and baby.
Types of Placenta Previa
Doctors generally classify placenta previa into two main categories based on how much of the cervix is covered:
Complete Placenta Previa occurs when the placenta entirely covers the cervical opening. This is the most serious form and almost always requires a cesarean section (C-section).
Partial Placenta Previa means the placenta covers only part of the cervix. Depending on how much of the cervix is involved, a vaginal delivery may or may not be possible.
Marginal Placenta Previa (sometimes called “low-lying placenta”) is when the placenta’s edge just reaches or barely grazes the cervix. Many cases of marginal previa resolve on their own as the uterus grows during the second and third trimesters.
What Causes Placenta Previa?
The exact cause isn’t always clear, but several factors are known to increase the risk:
- Previous uterine surgeries, including prior C-sections, fibroid removal, or D&C procedures, as scarring can affect where the placenta implants
- Advanced maternal age (over 35)
- Multiple pregnancies (twins, triplets, etc.)
- History of placenta previa in a previous pregnancy
- Smoking or cocaine use during pregnancy
- Being pregnant with a male fetus (slightly higher statistical association)
- In vitro fertilization (IVF)
It’s important to note that many women diagnosed with placenta previa have none of these risk factors. Sometimes, it simply happens.
How Is It Diagnosed?
Placenta previa is most often discovered during a routine second-trimester ultrasound, typically between weeks 18 and 20. If the placenta appears low-lying at this stage, your provider will schedule a follow-up ultrasound later in the pregnancy — usually around weeks 28 to 32 — to see if the placenta has moved.
Because the uterus grows significantly during pregnancy, what looks like previa early on often resolves on its own. In fact, up to 90% of low-lying placentas diagnosed in the second trimester migrate to a safe position by the third trimester as the lower uterine segment stretches upward.
If placenta previa is still present after 28 weeks, it’s considered persistent and is managed more closely. A transvaginal ultrasound (where a small probe is gently inserted into the vagina) may also be performed — it’s safe and gives a much clearer picture of the placenta’s exact position.
Signs and Symptoms to Watch For
The hallmark symptom of placenta previa is sudden, painless, bright red vaginal bleeding, typically occurring in the second or third trimester. This is sometimes called a “warning bleed.” Unlike other causes of pregnancy bleeding, the bleeding in placenta previa is usually:
- Painless (no cramping)
- Bright red in color
- Sudden in onset
- Potentially heavy
Some women experience repeated episodes of bleeding, while others may have no symptoms at all and the condition is found only on ultrasound.
Any vaginal bleeding during pregnancy should be reported to your healthcare provider immediately. Never assume it is harmless without evaluation.
How Does Placenta Previa Affect Pregnancy?
Placenta previa can impact pregnancy in several important ways:
Risk of Preterm Birth — Heavy bleeding may necessitate early delivery to protect the health of both mother and baby. Babies born early may face complications related to prematurity.
Placenta Accreta — Women who have placenta previa along with a history of uterine surgery (particularly C-sections) are at higher risk for placenta accreta, a serious condition where the placenta grows too deeply into the uterine wall and does not detach properly after delivery. This can lead to severe haemorrhage.
Anemia — Repeated bleeding episodes can deplete iron stores, leading to anemia in the mother, which may cause fatigue, weakness, and reduced oxygen delivery to the baby.
Fetal Malpresentation — Because the placenta occupies the lower uterus, the baby may not be able to settle into the head-down position, increasing the likelihood of a breech or transverse lie.
Emotional and Psychological Impact — Being placed on restrictions, facing uncertainty, and monitoring for bleeding can take a significant emotional toll. Anxiety and stress are common and completely valid responses.
How Is Placenta Previa Managed?
There is no treatment to move or reposition the placenta. Management focuses entirely on protecting the health of mother and baby until delivery is safe.
For Asymptomatic Cases (No Bleeding)
If placenta previa is diagnosed but causing no bleeding, your provider may advise:
- Pelvic rest — avoiding sexual intercourse, internal exams, and tampon use
- Activity restrictions — reducing strenuous physical activity
- Regular monitoring — more frequent ultrasounds and prenatal visits
- Avoiding long-distance travel, especially as the due date approaches
For Cases With Bleeding
If significant bleeding occurs, you may be admitted to the hospital for monitoring. Treatment may include:
- Bed rest in a hospital setting
- Blood transfusions if blood loss is severe
- Corticosteroid injections to help mature the baby’s lungs in case early delivery becomes necessary
- Tocolytic medications to slow or stop uterine contractions
Delivery Planning – Dr. Prajakta Sabale, Hinjewad
Placenta previa at term almost always calls for a planned C-section — the safest route for both mother and baby. Dr. Prajakta Sabale, the best gynecologist in Hinjewadi, typically plans the procedure around 36 to 37 weeks, ensuring the baby is mature enough while minimizing the risk of unexpected bleeding. Vaginal delivery is considered only in carefully selected marginal previa cases, and only after a detailed evaluation at her Hinjewadi clinic. With Dr. Sabale’s expertise, mothers receive a clear, personalized delivery plan — well in advance, with no surprises.
What to Expect After Delivery
For most women with placenta previa, the postpartum period is similar to recovery from any C-section. However, there is a higher risk of postpartum hemorrhage, so medical teams remain vigilant immediately after delivery.
In cases involving placenta accrete, surgery may be more complex, and in rare situations, a hysterectomy may be necessary to control bleeding and save the mother’s life. This is an outcome that medical teams work hard to anticipate and prepare for in advance.
Emotional Support Matters Too
A placenta previa diagnosis can turn what felt like a straightforward pregnancy into something filled with fear, uncertainty, and constant monitoring. It’s completely normal to feel anxious, frustrated, or even grief-stricken about the loss of a “normal” pregnancy experience.
Lean on your support system — partner, family, friends — and don’t hesitate to speak with a mental health professional if anxiety is becoming overwhelming. Online communities and support groups for high-risk pregnancies can also be tremendously helpful for connecting with others who truly understand what you’re going through.
Final Thoughts:
- Placenta previa occurs when the placenta covers part or all of the cervical opening, posing a risk of serious bleeding.
- Many cases detected early in pregnancy resolve on their own as the uterus grows.
- The key warning sign is sudden, painless, bright red vaginal bleeding — always report this immediately.
- Management depends on severity but typically involves pelvic rest, activity restrictions, close monitoring, and planned C-section delivery.
- With proper medical care, most women with placenta previa go on to deliver healthy babies.
- If you are experiencing any signs of placenta previa or have been diagnosed with a high-risk pregnancy, visit Dr. Prajakta Sabale at her clinic in Hinjewadi, Pune — one of the most trusted specialists for high-risk pregnancy treatment in the region. Early consultation can make your pregnancy journey safer, smoother, and stress-free.
This blog post is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. If you have concerns about your pregnancy, always consult your healthcare provider or obstetrician.